Efforts to personalise choice of initial therapy and any adjustments needed in cases of inadequate response are highly worthwhile. But we are at an early stage in our efforts to find biomarkers that distinguish likely responders from those less likely to benefit from a particular treatment.
Might longer be better?
Switching to an antidepressant with a different mechanism of action is often suggested when a patient does not respond adequately to one agent even after six to eight weeks of treatment. Work from the multinational Group for the Study of Resistant Depression (GSRD) challenged this view, according to Siegfried Kasper, Austria. It may be that staying with an antidepressant with the same mechanism of action for a longer period is more beneficial than switching.
Staying with an antidepressant with the same mechanism of action for a longer period is more beneficial than switching
More recently, the GSRD has been trying to develop a model that distinguishes between patients who do not respond adequately to a 6-8 week trial of one agent; treatment resistant depression, which is defined as non-response to adequate trial of two or more agents of different classes; and “chronic non-response”, the term used to categorize patients who have not been helped despite treatment with several antidepressants for more than twelve months.
Allelic combinations may predict response
A decade of work suggested that specific clinical features and individual single nucleotide polymorphisms (SNPs) provided little guidance to clinical outcome. This prompted the investigators to look at the interactions between clinical variables and SNPs in the hope that a pattern of features might prove more helpful.
They are currently suggesting that the absence of melancholia plus a set of three SNPs – the allelic combination of GG-GG-TT for rs6265, rs7430 and rs6313 of the BDNF, PPP3CC and HTR2A genes –might be such a combination. Around 62% of patients with these features showed a relevant HAM-D while only 34% of the study population as a whole responded to this extent.
Such studies, therefore, promise increasing ability to distinguish patients according to likelihood of response, but the large amount of data generated by this and other projects means that machine learning techniques are needed to handle it; and the output will be complex statistical algorithms.
Studies promise increasing ability to distinguish patients according to likelihood of response
Despite all we have learned about the variable aetiology and clinical presentation of depression, deciding between psychotherapy and pharmacotherapy, and prescribing a specific anti-depressant in an individual patient, largely remain a process of trial and error.
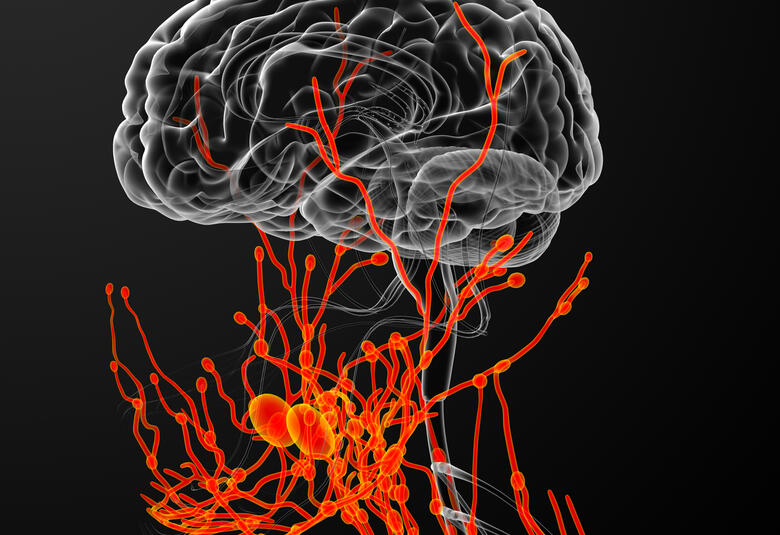
Imaging biomarkers for drug responses
Several fMRI studies suggested that greater baseline activity in the anterior cingulate cortex (ACC) and medial prefrontal cortex (mPFC) is associated with better response to SSRIs
There are still no widely accepted biomarkers to assist in making diagnosis more precise, nor in aiding choice of treatment in specific cases. So it perhaps not surprising that we seem stuck with response rates to drug treatment of 50% or less. Can neuroimaging, and functional MRI (fMRI) in particular, make a helpful contribution in this setting?, asked Shigeto Yawamaki, Japan.
Using tasks requiring response to emotional stimuli, several fMRI studies in patients with depression have suggested that greater baseline activity in the anterior cingulate cortex (ACC) and medial prefrontal cortex (mPFC) is associated with better response to SSRIs. In contrast, greater baseline activity in the amygdala seemed to predict better response to CBT.
Attention has recently focused on resting state fMRI as a means of investigating potential, clinically significant differences in brain circuitry underlying processing of reward and regulation of emotion. There is some evidence, for example, that treatment with SSRIs increases resting state connectivity between subcortical areas and the ACC. But, Professor Yawamaki cautioned, it is unlikely that any single clinical or imaging marker will adequately predict likelihood of response to specific kinds of intervention or classes of antidepressant.
Our correspondent’s highlights from the symposium are meant as a fair representation of the scientific content presented. The views and opinions expressed on this page do not necessarily reflect those of Lundbeck.